HIP REPLACEMENT SURGERY
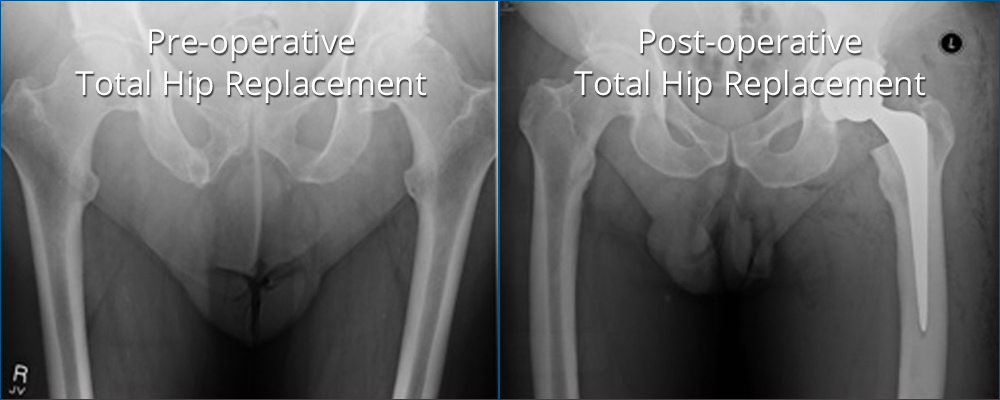
As the name suggests, hip replacement surgery replaces the worn out hip joint with a prosthetic (artificial) joint. Total hip replacement, although dating back to the 1940’s, was advanced in the UK in the 1950’s and 60’s by Sir John Charnley. Today, over 55,000 total hip replacements are performed in the UK each year. There are now many different types of hip replacement available. The most widely used consist of a metal ball articulating with a plastic socket. Some hip replacements are designed to be used with orthopaedic cement, which acts as a grout; others are designed to encourage bone growth onto the prosthesis to give long term stability (uncemented).
It is the plastic liner that wears out with time, probably related to activity levels. Technological advances, however, have produced bearing surfaces which can withstand higher activity levels and will therefore wear out more slowly. These newer bearing surfaces are either metal-on-metal or ceramic-on-ceramic. Patients who are young and physically active may benefit from these newer hip replacements since the risk of implant failure is reduced.
HIP RESURFACING
Recent attention has focussed on Hip Resurfacing. Here, the acetabulum (socket) is replaced with a metal cup and the femoral head (ball) is shaped to allow a metal surface replacement to be implanted.
Hip resurfacing has the potential benefit of preserving femoral bone; the use of a metal-on-metal bearing couple should reduce the amount of wear and therefore increase implant survival.
However the long-term effects of metal-on-metal bearing surfaces have been shown to cause high levels of (cobalt and chromium) metal ions in the blood. These metal ions have been linked to some forms of cancer (particularly lymphomas and leukaemias). Although there is no proof that the risk of these cancers is increased in patients with hip resurfacing, these findings have caused concern amongst orthopaedic surgeons.
Other potential problems with hip resurfacing are the risk of fracture of the femoral neck (1-3%) and the need to remove more bone from the pelvis than a conventional hip replacement to allow the cup to be inserted. The scar from a hip resurfacing procedure is much larger than that for a conventional hip replacement and the operation usually takes longer. Recovery for both operations is very similar.
Whilst knowledge of the options available is useful to patients, the surgeon should choose the most appropriate type of hip replacement for each patient.
WHAT ARE THE BENEFITS OF HIP REPLACEMENT?
The majority of patients experience the following benefits following hip replacement:
- Abolition or at least a significant reduction in hip pain
- Improvement in life quality
- Return to normal daily activities and low impact sports
- Sleeping without pain
- Improvement in leg strength as a result of a return to more normal levels of activity
- Years of reliable function.
THE PROCEDURE
THE NEW MINIMALLY INVASIVE HIP REPLACEMENT TECHNIQUE
Mr Aslam now offers a minimally invasive, tissue sparing, total hip replacement using a new technique.
By not cutting any muscles around the hip and working through a small ‘window’ in the tissues, the hip can be replaced with minimal soft tissue damage. This can provide faster recovery, shorter hospital stay and rapid return to full function.
With the new minimally invasive Hip Replacement surgery there is no surgical dislocation of the hip. By not surgically dislocating the hip, there is less trauma to the surrounding muscles and tendons and no muscles are cut during surgery.
With this technique, the implant is built inside the body, so the hip is not twisted into unnatural positions. This leaves more tissue intact, specifically the short external rotator tendons and gluteus medius muscle. These muscles are normally responsible for preventing dislocation.
Read more about minimally invasive hip replacement surgery here.
Discussion with Nadim is important to answer any questions that you may have. For information about any additional conditions not featured within the site, please contact us for more information.










